How It Works
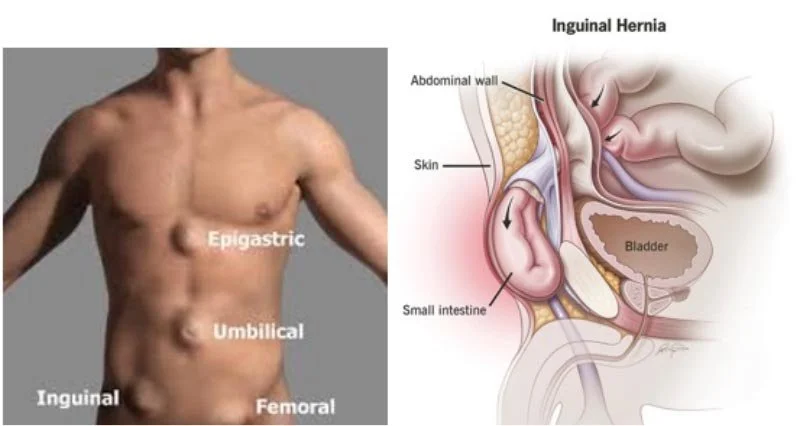
A hernia occurs when of the body’s organs pushes through the muscle or tissue that contains it. This usually occurs in the abdomen or groin. Common types of hernia are shown in Figure 2. Hernias can occur as people get older and muscles begin to weaken; they can also result from a birth defect. An inguinal hernia occurs in the groin area when abdominal tissues, or part of the small intestine, protrude into an opening in the abdominal wall (the inguinal canals). Inguinal hernia repair is one of the most common types of surgery in the world: there are an estimated 20 million groin hernia repair surgeries performed annually.
Figure 2. (Left) Common types of hernia. (Right) Inguinal hernia.
There are two types of inguinal hernia: direct inguinal hernias penetrate directly though the wall of the inguinal canal; indirect inguinal hernias enter the inguinal canal from the top.
Inguinal hernia is much more common in men than women. About 90% of repair surgeries are performed in men [i]; the estimated lifetime risk of inguinal hernia in men is 27% and 3% in women [ii]. Occurrence is most common in people ages 75 to 80 [iii].
Not all hernias require immediate treatment, but most eventually do since they usually worsen over time. Hernias create bulges where the tissue presses outward and cause unpleasant symptoms including pressure, discomfort, and pain. In males, the hernia can slip into the scrotum and cause swelling, pain during sex, and other issues [iv]. If left untreated, hernias can cause serious health complications, such as infection and/or loss of blood to the intestine [v].
Currently, there are three types of surgery performed for inguinal hernia repair:
Open (traditional) surgery: A single incision is made to expose the herniated tissue. The surgeon puts the organs and tissue back into place and stitches the tissue back together, often with surgical mesh used as a reinforcement.
Laparoscopic hernia repair surgery: Also known as “keyhole surgery”. The surgeon uses 3-4 small incisions to operate. A thin lighted tube with a video camera (laparoscope) is used to visualise the inside of the body through one of the incisions, while instruments are inserted into the other incisions to repair the hernia.
Robotic hernia repair surgery: A laparoscopic surgery performed with robotic surgical instruments that the surgeon operates from a console [vi].
Open surgery is the oldest technique and is the most invasive. As a minimally invasive procedure, laparoscopic hernia repair gained popularity in the 1990s as it provided lower postoperative pain and faster recovery than open surgery. Robotic laparoscopic surgery is still relatively new, with its first use in humans in 2007. It allows surgeons to view three-dimensional images of the body, and reduces scar size, pain, and recovery time.
Despite the advances in hernia repair, 13% of all groin hernia repairs are performed for recurrent hernias [vii]; 10-12% of patients suffer from chronic pain following primary inguinal hernia repair [viii]. For the 20 million patients who undergo groin hernia repair each year, 2.6 million have this procedure performed because their hernia came back and between 2 and 2.4 million have chronic pain following surgery.
There is no consensus regarding standardised therapy for inguinal hernia, even among professional societies. Since mesh augmentation was introduced, many different techniques have been developed, each with their own risk factors [ix]. The materials used in hernia repair can also cause problems. Mesh is used in around 80% of inguinal hernia repair procedures [x], with the Lichtenstein “tension free” mesh technique, developed in 1984 still considered the gold standard of hernia repair [xi] [xii]. Mesh is used to strengthen the repair and reduce recurrence.
Figure 3. Infection following bilateral inguinal hernia repair. https://doi.org/10.1186/s12879-023-08039-9.
Mesh may either be synthetic or made from animal tissue. Mesh made from animal tissue is absorbable, allowing for natural tissue growth, while synthetic mesh may either be absorbable or non-absorbable (and therefore a permanent implant). Regardless of composition, the insertion of mesh can trigger an immune response and result in the body’s rejection of the mesh, although this is more common with synthetic mesh [xiii].
In the US from 2005 to 2021, over 211,000 of hernia procedures that involved the use of mesh devices exhibited complications. Subsequently, various meshes were removed from the US market during the same period for issues including high failure rate and complications including adhesions, bowel fistulas, punctured organs, device migration, and bowel obstruction. More than 26,000 lawsuits have been filed against Johnson & Johnson’s Ethicon, Bard Davol, Atrium, and Covidien due to mesh related issues [xiv].
Current Specification
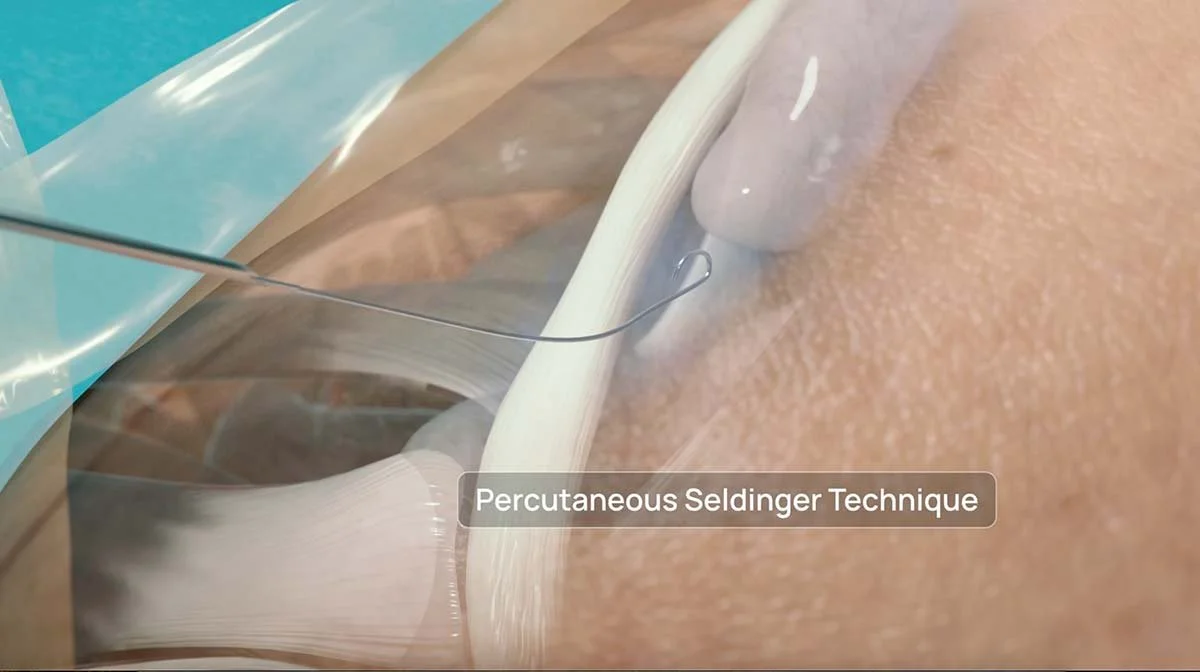
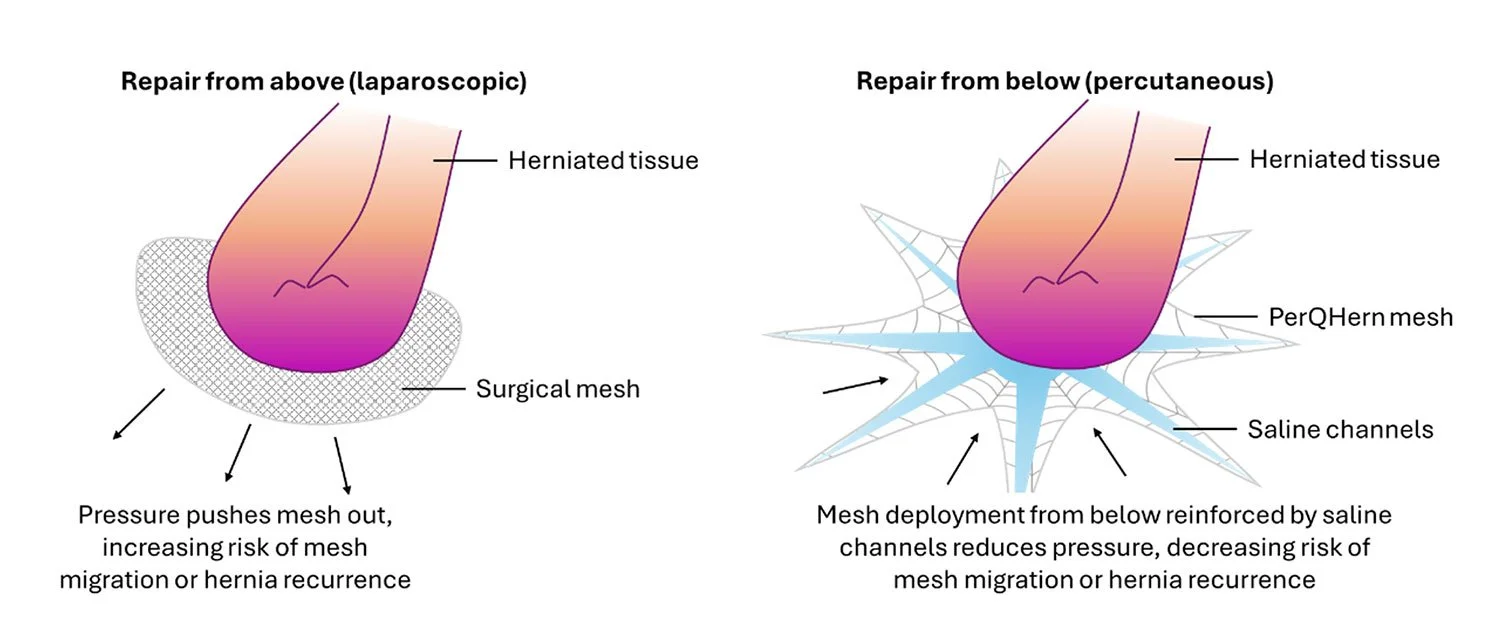
A truly gold standard medical device for inguinal hernia repair would (i) use a percutaneous delivery system to avoid the need for surgical incisions with (ii) a novel mesh design that does not weaken over time and reduces the risk of infection, chronic pain, and hernia recurrence and (iii) avoids the need for fixation on the abdominal floor without risk of migration, (iv) enabling the procedure to be performed in an outpatient setting without general anaesthesia in 20 minutes or less.
Unsatisfied Need
There is no percutaneous solution for inguinal hernia repair available on the market today, with most repairs completed with a mesh technique developed over 40 years ago. As a result, the current methods can require time to recover from the incisions, cause pain, and recurrence of the hernia. In addition, hernia mesh device recalls have plagued patients, physicians, and the healthcare systems with high failure rates and significant complications. As inguinal hernia operations are one of the most common surgical procedures performed in the world, there is a clear and urgent unmet need for an inguinal hernia repair system that provides the support needed to strengthen the repair, prevent recurrence, and reduce pain and recovery time. Any meaningful innovation in the treatment of the 20 million people who undergo groin hernia repair annually would provide a massive, market altering impact to surgeons, health care systems, and patients through the reduction of recurrence and chronic pain.
Product Offering
PerQHern is the world’s first percutaneous inguinal hernia repair system. As the first of its kind, it is the only method of inguinal hernia repair that meets the gold standard for this type of treatment:
Uses a percutaneous delivery system to avoid the need for surgical incisions
Has a novel mesh design that does not weaken over time and reduces the risk of infection, chronic pain, and hernia recurrence
Avoids the need for fixation on the abdominal floor without the risk of migration
Enables the procedure to be performed in an outpatient setting without general anaesthesia in 20 minutes or less
As a result of meeting all four elements of the specification, PerQHern has the potential to reduce hernia recurrence rates for patients undergoing inguinal hernia repair to as low as 3%, compared to the current recurrence rates of 13% for open surgical and laparoscopic repairs. Worldwide, this would save approximately 2 million hernia recurrences for the 20 million inguinal hernia repair procedures performed annually.
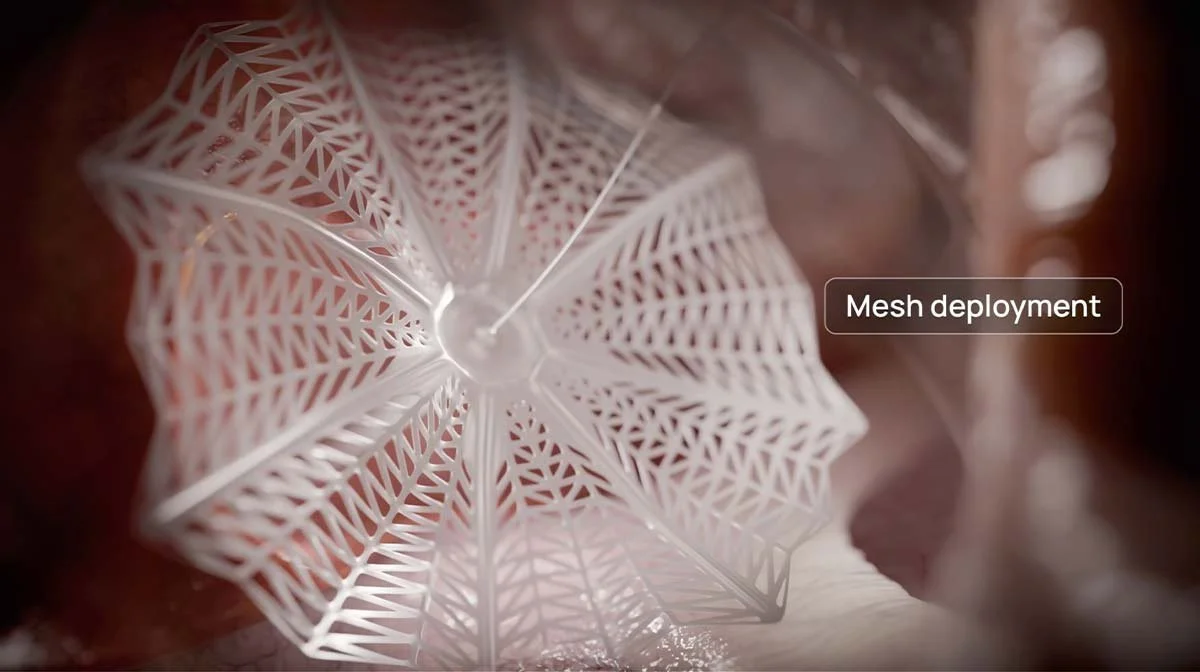
Product Technique
The technique is based on biomimicry and utilizes the distribution of radial force and structural integrity of a spider’s web. Rather than using a conventional woven mesh, PerQHern’s device adopts a novel computer-guided laser cutting of PTFE with a custom matrix to provide a homogenous distribution of adhesion and even resistance to centripetal forces.
Once available, it is envisaged that patients will opt to undergo a percutaneous bespoke implant procedure rather than currently available multiport laparoscopic incision surgery or open surgery.
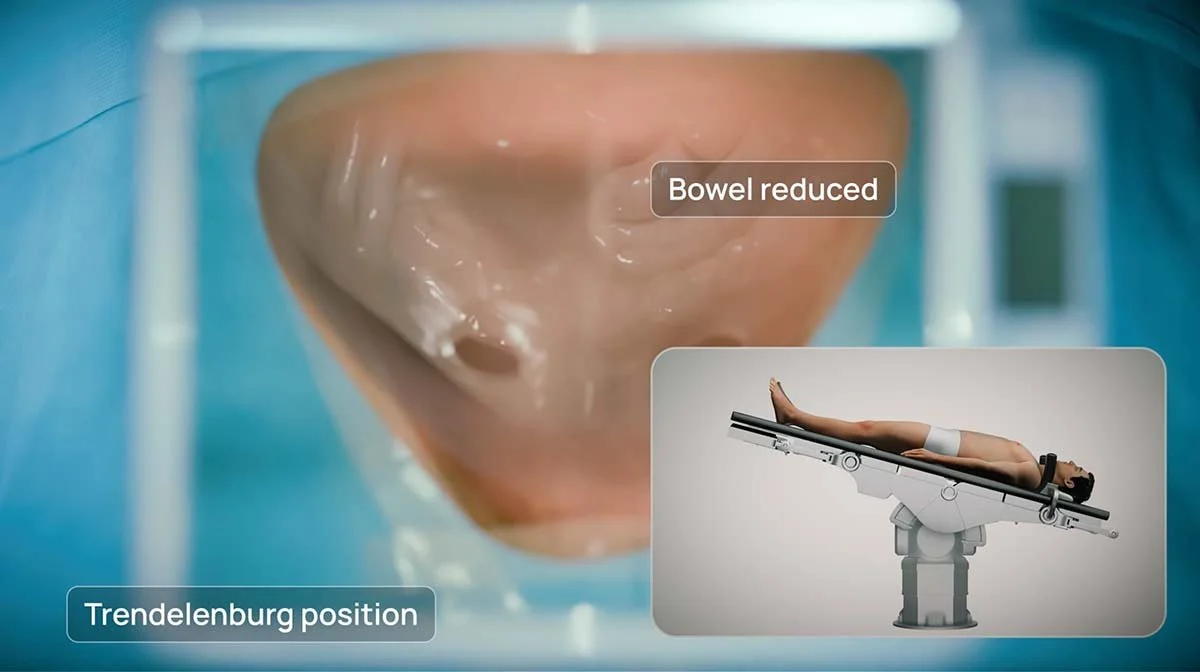
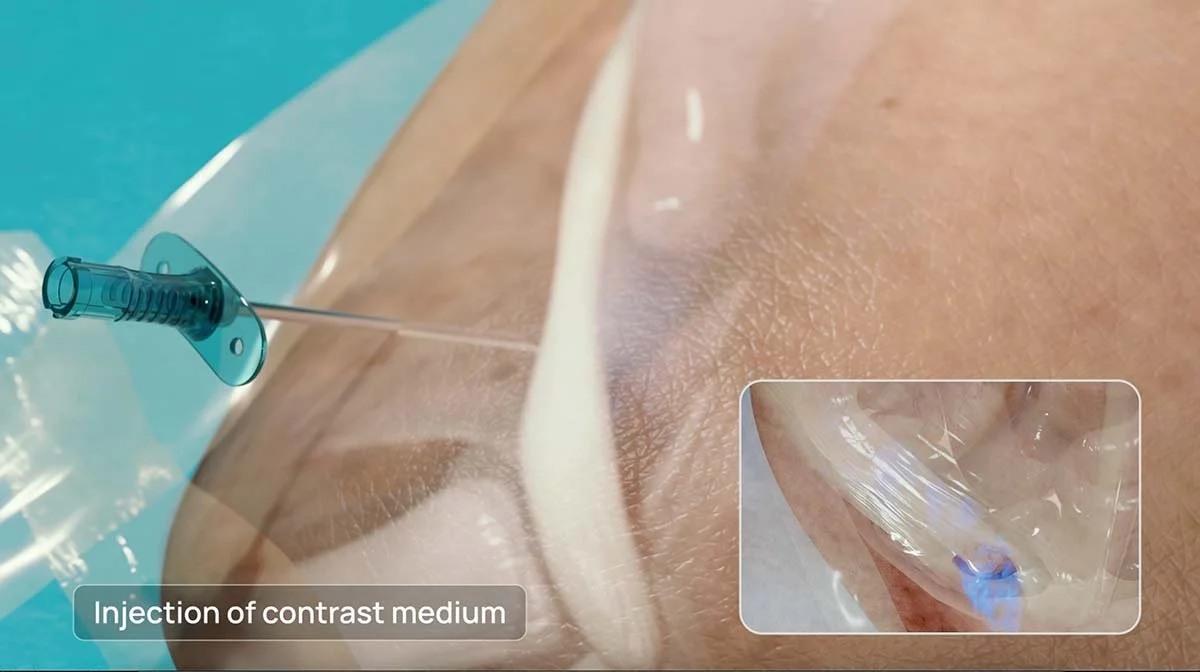
The stages of the PerQHern delivery are described below Figure 4:
Figure 4. Sequential steps of the PerQHern delivery.
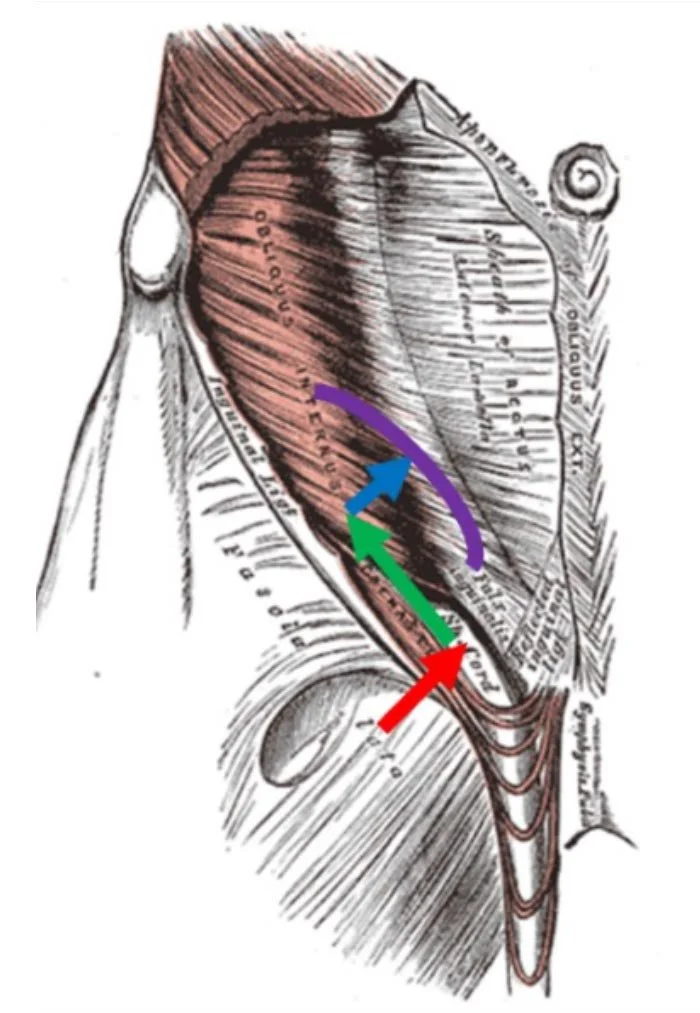
After passing through the skin, PerQHern's sheath will enter the inguinal canal through the superficial inguinal ring (inverted V) directly medial to the pubic crest.
PerQHern's sheath and delivery system will advance along the inguinal canal and then free-up the peritoneal sac adhesions from the spermatic cord and canal wall.
After the peritoneal adhesions in the inguinal canal have been freed, PerQHern's sheath will then enter the abdominal cavity through the deep internal inguinal ring but external to the peritoneum.
After the bowel has been pushed up and away by a parasol balloon, the mesh will be inflated and expanded in place covering the deep inguinal ring.
PerQHern’s percutaneous inguinal hernia repair system:
Watch the full Video below:
As a result, PerQHern’s system will reduce hospital costs including theatre time, staff numbers, general anaesthesia, and post-operative costs. With the costs of operating room time estimated at €560 per hour in Ireland [xxiv], moving the procedure to an outpatient setting will save between €280 (for a 30-minute procedure) and €420 (for a 45-minute procedure) in these costs alone. For patients, repair with PerQHern will improve healing time, reduce pain, and provide a more durable hernia repair with less chance of recurrence.
References:
[i] Agarwal PK. Study of Demographics, Clinical Profile and Risk Factors of Inguinal Hernia: A Public Health Problem in Elderly Males. Cureus. 2023 Apr 24;15(4):e38053. https://doi.org/10.7759/cureus.38053. PMID: 37122980; PMCID: PMC10132853.
[ii] Ibid.
[iii] American Society of Anesthesiologists. Hernia Surgery. https://madeforthismoment.asahq.org/preparing-for-surgery/procedures/hernia-surgery/. Accessed 21 January 2025.
[iv] Cleveland Clinic. (21 September 2023) Hernia Repair Surgery. https://my.clevelandclinic.org/health/procedures/17967-hernia-repair-surgery. Accessed 21 January 2025.
[v] MedStar Health. (26 May 2021) Mesh and No Mesh Hernia Repair. https://www.medstarhealth.org/blog/hernia-mesh-and-no-mesh-repair. Accessed 21 January 2025.
[vi] Cleveland Clinic. (21 September 2023) Hernia Repair Surgery. https://my.clevelandclinic.org/health/procedures/17967-hernia-repair-surgery. Accessed 21 January 2025.
[vii] Sharma A, Sarwal A. Surgical repair in recurrent inguinal hernia. Ann Laparosc Endosc Surg 2017;2:97. https://doi.org/10.21037/ales.2017.05.03.
[viii] Köckerling F, Simons MP; Current Concepts of Inguinal Hernia Repair. Visc Med 24 April 2018; 34 (2): 145–150. https://doi.org/10.1159/000487278.
[ix] Weyhe, D., Tabriz, N., Sahlmann, B., & Uslar, V. N. (2017). Risk factors for perioperative complications in inguinal hernia repair - a systematic review. Innovative surgical sciences, 2(2), 47–52. https://doi.org/10.1515/iss-2017-0008.
[x] Baylón, K., Rodríguez-Camarillo, P., Elías-Zúñiga, A., Díaz-Elizondo, J. A., Gilkerson, R., & Lozano, K. (2017). Past, Present and Future of Surgical Meshes: A Review. Membranes, 7(3), 47. https://doi.org/10.3390/membranes7030047.
[xi] Kapoor, VK. (18 Apr 2023). Open Inguinal Hernia Repair. Medscape. https://emedicine.medscape.com/article/1534281-overview?form=fpf. Accessed 22 January 2025.
[xii] UCLA Health. Lichtenstein Tension-Free Hernia Repair. https://www.uclahealth.org/medical-services/surgery/hernia-care/hernia-repair/lichtenstein-tension-free-hernia-repair. Accessed 22 January 2025.
[xiii] MedStar Health. (26 May 2021) Mesh and No Mesh Hernia Repair. https://www.medstarhealth.org/blog/hernia-mesh-and-no-mesh-repair. Accessed 21 January 2025.
[xiv] Sarmiento, S, Turner, T. (16 December 2024). Hernia Mesh Recalls. Drugwatch. https://www.drugwatch.com/hernia-mesh/recalls/#:~:text=As%20of%20the%20latest%20update,no%20longer%20on%20the%20market. Accessed 22 January 2025.
[xv] NHS. (15 October 2021). How it’s performed: Inguinal hernia repair. https://www.nhs.uk/conditions/inguinal-hernia-repair/what-happens/.
[xvi] Weyhe, D., Tabriz, N., Sahlmann, B., & Uslar, V. N. (2017). Risk factors for perioperative complications in inguinal hernia repair - a systematic review. Innovative surgical sciences, 2(2), 47–52. https://doi.org/10.1515/iss-2017-0008.
[xvii] Sarmiento, S, Turner, T. (16 December 2024). Hernia Mesh. https://www.drugwatch.com/hernia-mesh/ Accessed 10 February 2025.
[xviii] Ibid.
[xix] Wilson, R. B., & Farooque, Y. (2022). Risks and Prevention of Surgical Site Infection After Hernia Mesh Repair and the Predictive Utility of ACS-NSQIP. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract, 26(4), 950–964. https://doi.org/10.1007/s11605-022-05248-6.
[xx] Zamkowski, M., Śmietański, M. (2023) MEsh FIxation in Laparoendsocopic Repair of Large M3 inguinal hernias: multicenter, double-blinded, randomized controlled trial—study protocol for a MEFI Trial. Trials 24, 572. https://doi.org/10.1186/s13063-023-07601-9.
[xxi] Ibid.
[xxii] NHS. (15 October 2021). How it’s performed: Inguinal hernia repair. https://www.nhs.uk/conditions/inguinal-hernia-repair/what-happens/.
[xiii] Wilson, R. B., & Farooque, Y. (2022). Risks and Prevention of Surgical Site Infection After Hernia Mesh Repair and the Predictive Utility of ACS-NSQIP. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract, 26(4), 950–964. https://doi.org/10.1007/s11605-022-05248-6.
[xxiv] O'Donnell, B. D., Walsh, K., Murphy, A., McElroy, B., Iohom, G., & Shorten, G. D. (2017). An evaluation of operating room throughput in a stand-alone soft-tissue trauma operating theatre. Romanian journal of anaesthesia and intensive care, 24(1), 13–20. https://doi.org/10.21454/rjaic.7518.241.wal.